Øystein Brorsons borreliaforskning: Intelligent nysgjerrighet og utfordrende funn
Det personlige engasjementet som Øystein Brorson la ned i borreliadiagnostikken var imponerende. Han kunne sikkert både irritere og provosere, og noen ganger ble hans vurderinger i en klinisk infeksjonsmedisinsk sammenheng litt vel spenstige.
Fra BIOINGENIØREN.
PUBLISERT
ENDRET
Jeg er likevel overbevist om at publikasjonene hans har gitt viktig kunnskap som det vil bli bygget videre på, skriver hans mangeårige samarbeidspartner, pensjonert overlege Per Bjark, i denne kronikken om Brorsons arbeid.
Burgdorfers funn
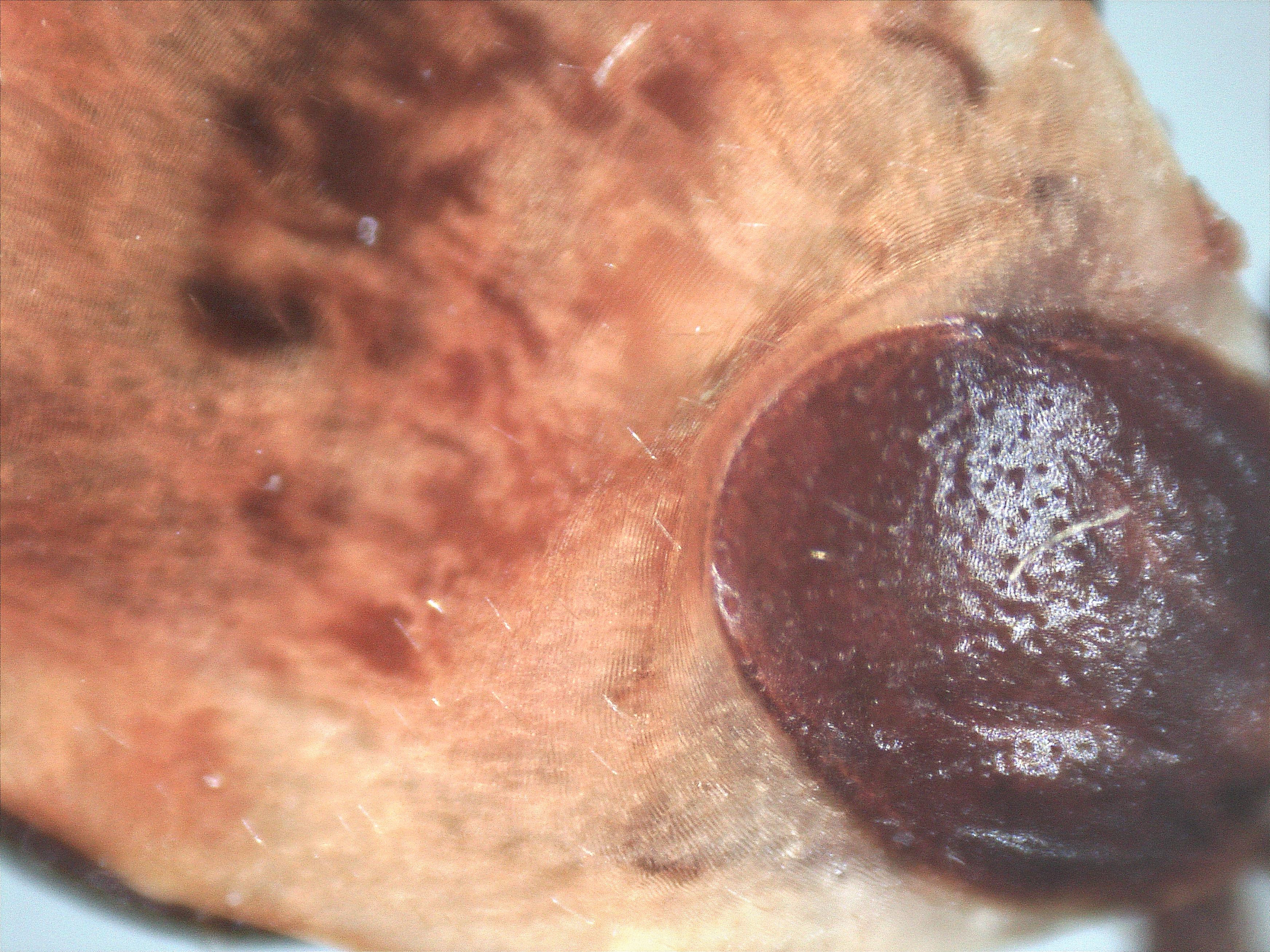
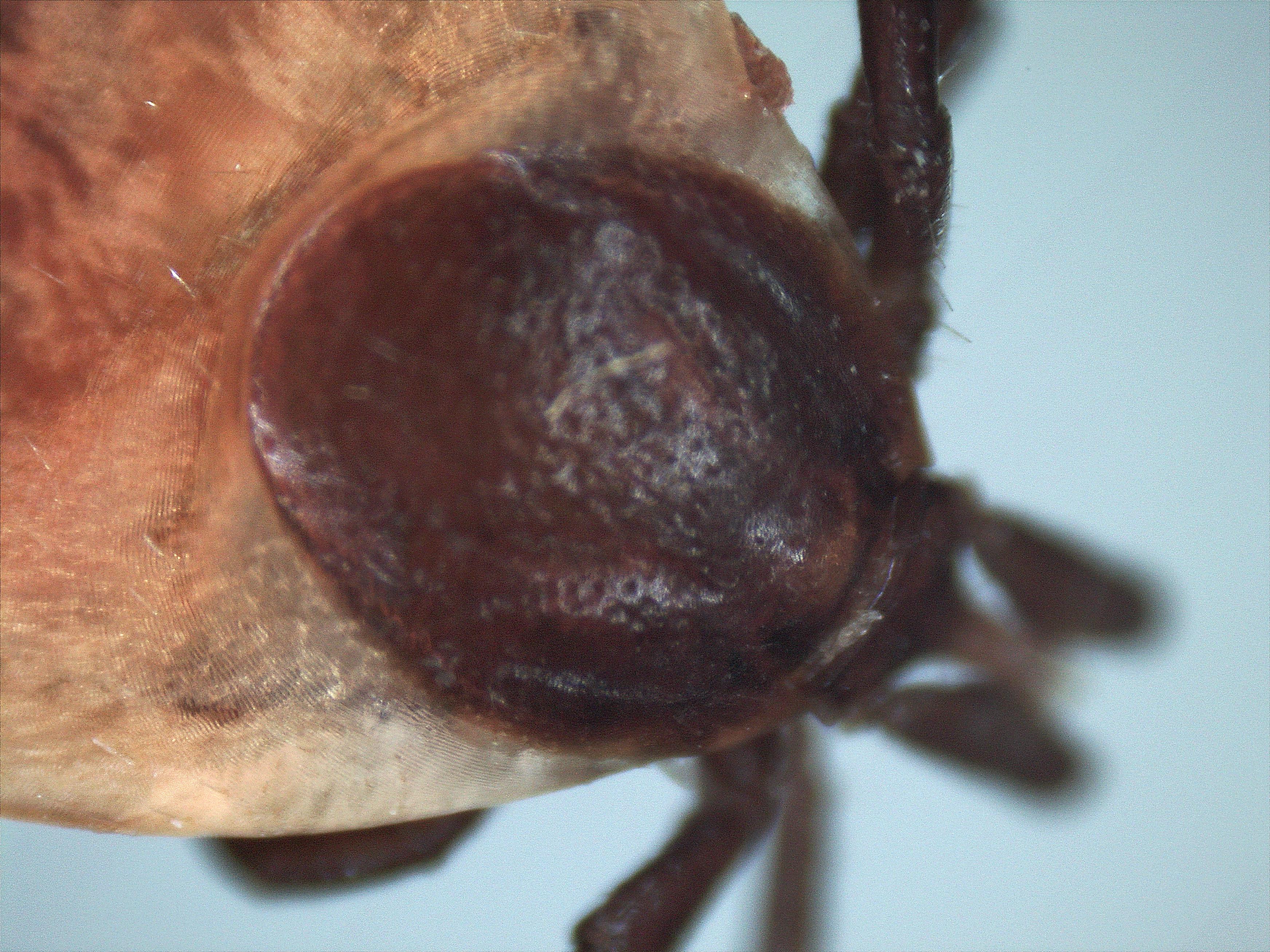
Det var i USA, på 1970-tallet, at tilstanden som senere fikk navnet Lyme borreliose, ble fastslått å være en flåttbåren infeksjonssykdom. I begynnelsen var man opptatt av leddmanifestasjonene, men det ble raskt dokumentert at det dreide seg om en multiorgansykdom. Flere elementer i sykdomsbildet er i virkeligheten beskrevet for mer enn 100 år siden, uten at man da visste årsaken.
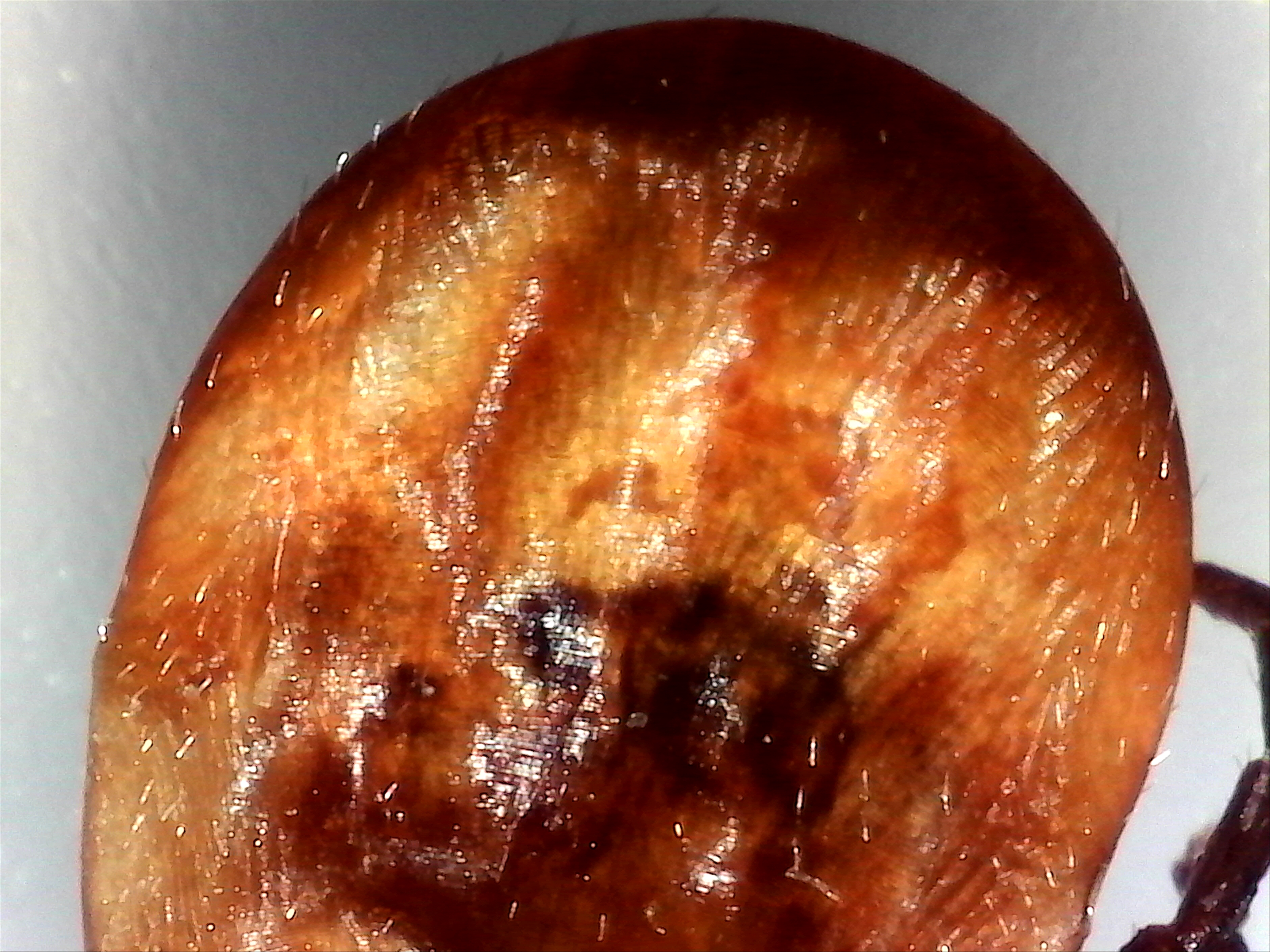
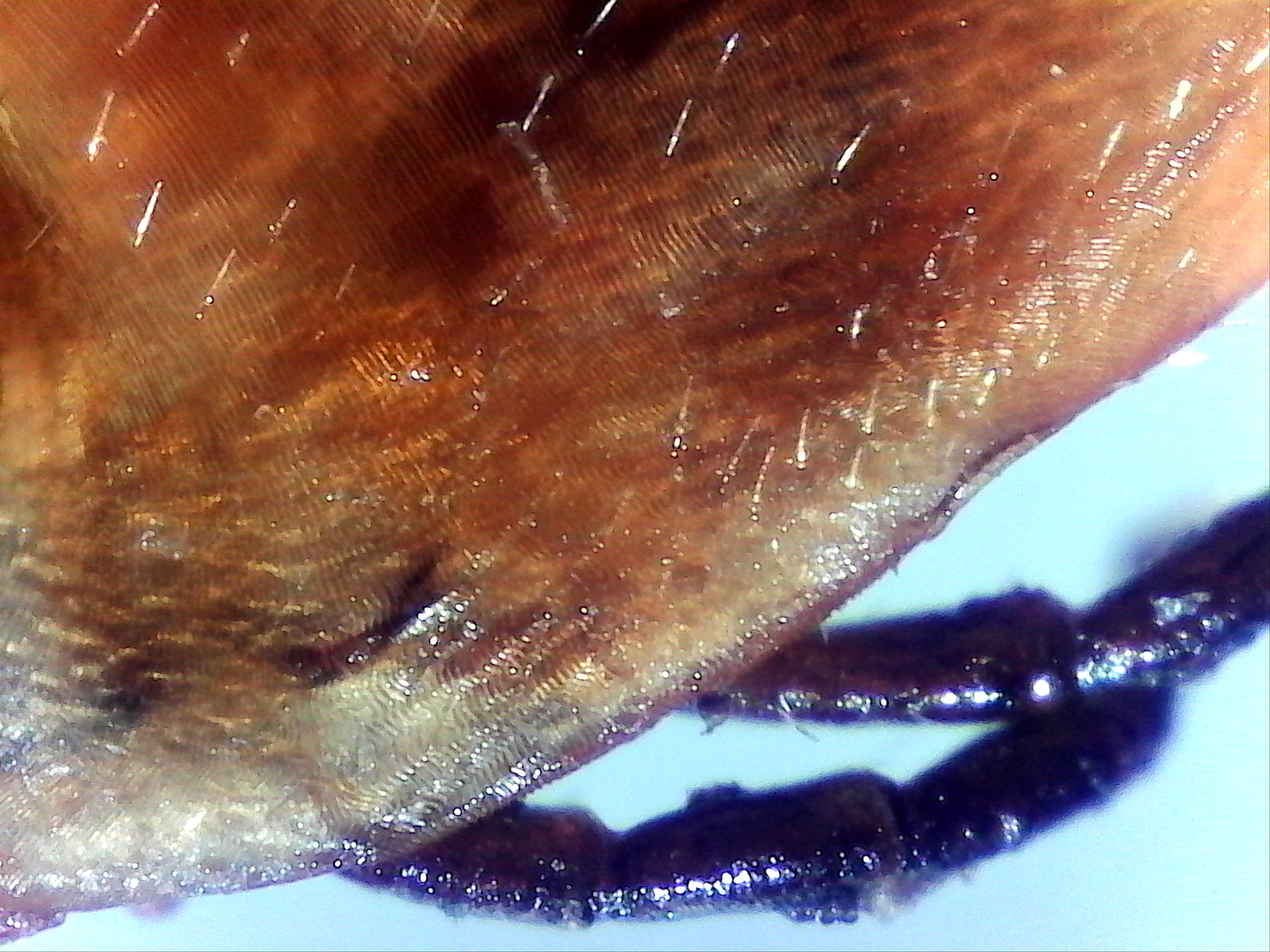
Bakterien som var årsaken til sykdommen ble isolert av biologen Willy Burgdorfer i Montana. Da han i 1982 studerte flått fra østkysten av USA, fant han overraskende spiralformede bakterier, spirocheter, i flåttens tarmsystem. Man forsto raskt at dette var årsaken til ”Lyme disease” (1). Bakterien ble oppkalt etter Burgdorfer.
Det er nå kjent omtrent et dusin undertyper av Borrelia burgdorferi sensu lato (s.l.). I USA er det bare B. burgdorferi sensu stricto (s.s.) som er av humanmedisinsk betydning. I Europa finnes flere underarter av B. burgdorferi s.l.. Viktigst er den typisk skandinaviske B. afzelii, samt B. garinii som har størst utbredelse i Mellom-Europa. I tillegg har også Europa en del B. burgdorferi s.s.. B. valaisiana, B. spielmanii, B. lusitaniae, m.fl er påvist mye sjeldnere. Spirochetene kan invadere flere typer vev og organer, blant annet hud, nervesystem, ledd, muskler, sener, hjerte og øyne.
Diagnostiske utfordringer
Jeg tror Øystein Brorson var fascinert av det mangslungne i spirochetebiologien og de mangeartede utslag infeksjonene kunne gi. I tillegg leste han seg hele tiden opp på de mange egenskaper Borrelia burgdorferi etter hvert ble dokumentert å ha. Han så også tidlig den store utfordringen laboratoriene hadde når de skulle bekrefte Lyme borreliose av forskjellige typer og i forskjellige stadier.
I en oversiktsartikkel i Bioingeniøren i 2007 (2) redegjorde han for historikken, de viktigste underartene, bakteriens rikholdige genetiske utrustning, de mange egenskapene som bidrar til sykdomspanoramaet, bakteriens evne til å motstå våre normale forsvarsmekanismer mot infeksjon, og ikke minst de diagnostiske utfordringene.
Diagnostikken utvikles
I motsetning til syfilisspirocheten, lot B. burgdorferi seg dyrke i laboratoriet. Et spesialmedium ble tidlig på 1980-tallet utviklet i USA. Øystein Brorson fikk noen år senere tilsendt en borreliakultur som han holdt gående i årevis og som han brukte til laboratorieeksperimentene sine. Diagnostikk basert på vår immunrespons ble tidlig utviklet både i Norge, Sverige og Danmark, men det var vanskelig å få til en tidlig og treffsikker påvisning.
Nevrologen Bodvar Vandvik ved Rikshospitalet, var en pioner i internasjonal sammenheng på midten av 1980-tallet når det gjaldt immunoblot for antistoffpåvisning hos nevrologiske pasienter. Det kom også tidlig viktige bidrag fra Sverige, samtidig som man så at det var mange svakheter ved de kommersielt tilgjengelige testene. Brorson undersøkte flere leverandørers tester og bekreftet at det var betydelige forskjeller. Han bidro sterkt til at man ved sykehuset i Tønsberg tidlig gjorde et heldig valg blant testtilbudene. Samtidig erfarte man at det tok tid før målbar immunrespons kunne bekreftes i de tilgjengelige testene ved tidlige faser av Lyme borreliose. Professor Schutzers gruppe i New Jersey undersøkte såkalte immunkomplekser ved Lyme borreliose (3). Dette var en metode Øystein Brorson tok opp og som senere kom til å få en stor plass i vårt kliniske arbeid ved Sykehuset i Vestfold. Det ble også gjort interessante observasjoner ved flere universiteter i Mellom-Europa. Alt i alt var det mange utfordringer. Vi hadde planene klare for en observasjonell etterundersøkelse av en pasientgruppe med tunge immunkompleksutslag, da Øystein brått ble syk og satt ut av spill i april 2010.
Fettere og forskerkolleger
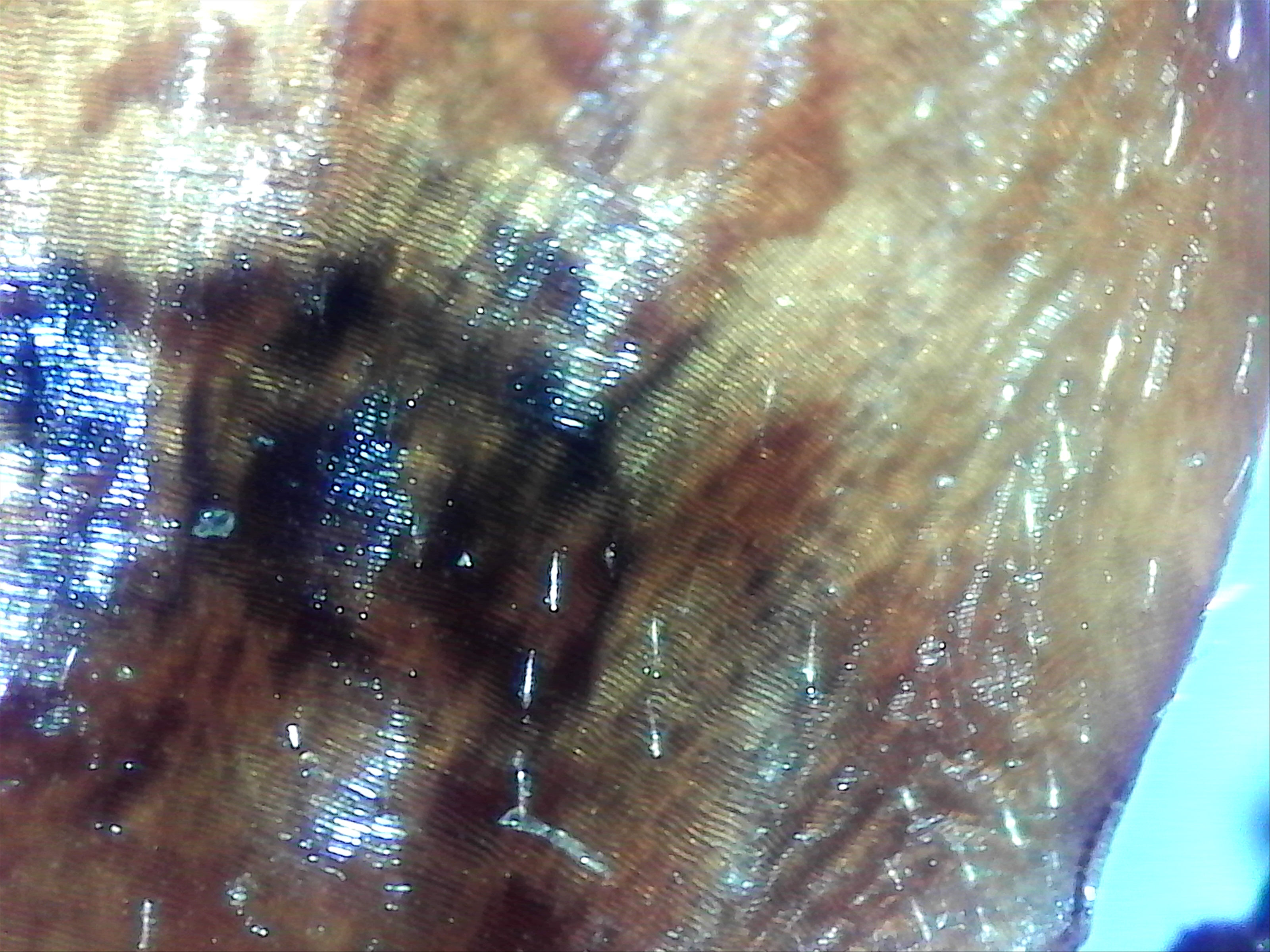
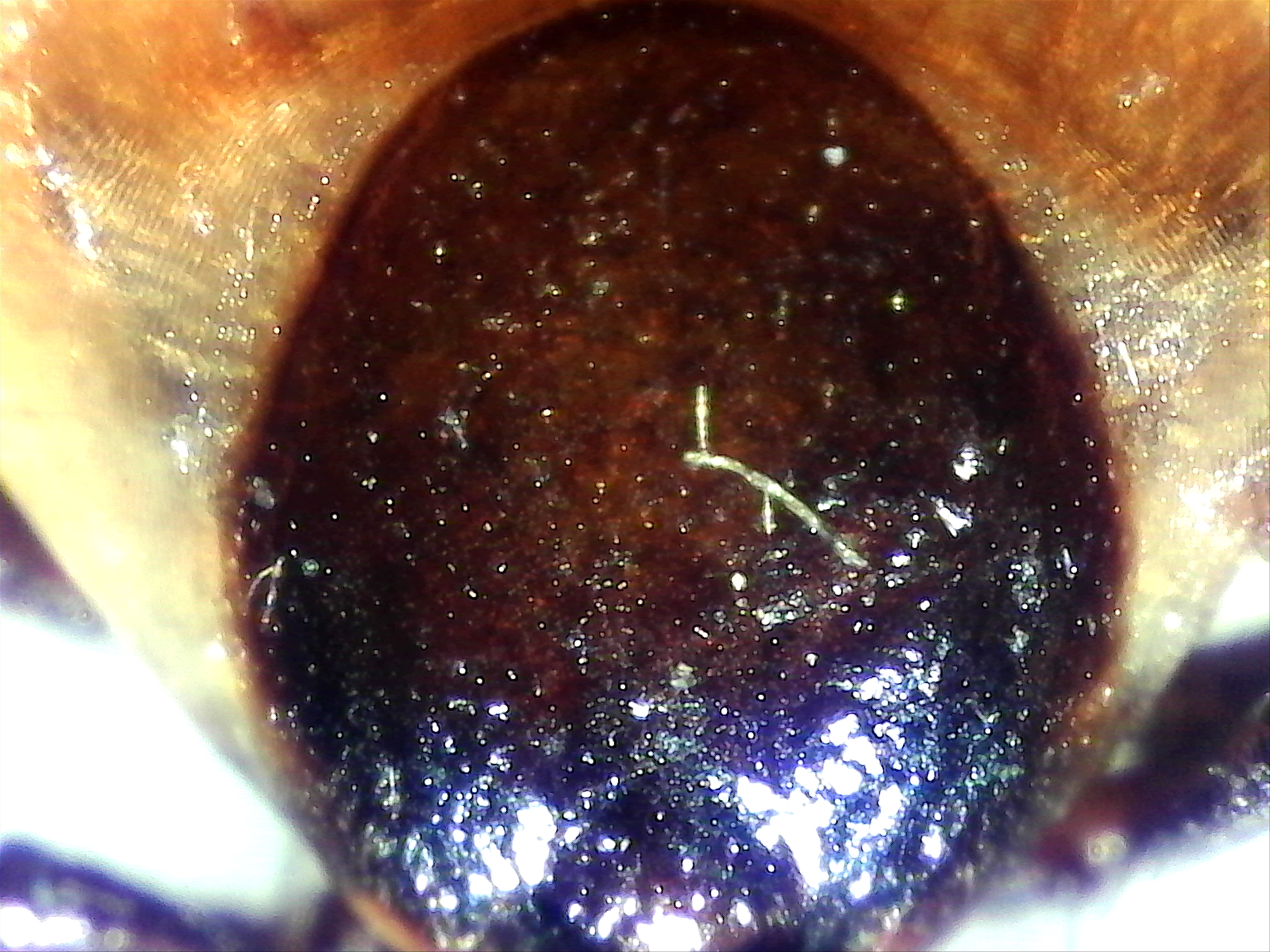
I borreliakulturen som Brorson holdt gående på sitt arbeidssted ved Mikrobiologisk avdeling, Sykehuset i Vestfold, observerte han strukturelle endringer ved bakterien. Dette ble fulgt opp med flere undersøkelser (4, 5, 6). Vanlig lysmikroskopi kunne dokumentere noe, men i samarbeid med sin fetter, Sverre-Henning Brorson, som var ekspert på elektronmikroskopi og hadde tilgang til denne metode på sitt arbeidssted i Oslo, ble det gjort bemerkelsesverdige observasjoner. Brorson brukte de første årene betegnelsen ”cyster” på de små overlevelsesformene av B. burgdorferi, nå kalles de like gjerne ”round bodies” (7). Samarbeidet mellom de to forskerne og slektningene ble avgjørende for publisering og internasjonal oppmerksomhet. Øystein hadde i begynnelsen vanskeligheter med å få sine artikler trykket i internasjonale tidsskrifter, men da de først kom, ble de lagt merke til.
Da Brorson møtte Burgdorfer
Artikkelen som Øystein og Sverre-Henning Brorson publiserte i 1997, ble et avgjørende bidrag (4). Øystein hadde da fått til å utvikle «cystene” til bevegelige, normale spirocheter ved å optimalisere betingelsene i kulturen, mens fetteren skaffet den tunge elektronmikroskopiske dokumentasjonen. Jeg husker godt Burgdorfers åpningsforedrag ved den internasjonale konferansen om Lyme borreliose i München i 1998, da han roste ”the very interesting contributions from Norway”. Det var Brorson & Brorsons publikasjoner han siktet til. Øystein var til stede på kongressen og hadde med en poster med detaljer fra de morfologiske undersøkelsene de hadde gjort. Det fant sted en lang og ivrig diskusjon mellom Burgdorfer og Øystein foran posteren. Øystein var svært oppglødd etterpå. Han hadde tidligere møtt mye skepsis og hatt vanskeligheter med å få publisert det mange mente bare var uinteressante laboratorieartefakter. Nå møtte han stor anerkjennelse fra selveste Willy Burgdorfer!
Hans arbeider fant også støtte i publikasjoner fra andre vitenskapelige miljøer, ikke minst professor Marina Cinco ved universitetet i Trieste (8). I USA var man (og er fortsatt) mer lunkne. I en ganske fersk publikasjon fraskriver man utrolig nok disse persistensformene enhver betydning (9).
Sirkulerende immunkomplekser
Personlig mener jeg at Brorson gjorde en annen meget viktig oppdagelse da han påviste effekt av metronidazol på de cystiske formene av B. burgdorferi (6). Fremdeles mangler vi her gode kliniske data, men med støtte i Brorsons laboratoriefunn, har undertegnede latt en del Lyme borreliosepasienter med utilfredsstillende forløp etter vanlig primærbehandling, bli rebehandlet med metronidazol, i tillegg til et helt konvensjonelt middel som de hadde fått i første omgang. Vi kunne konstatere god klinisk effekt hos flere. Dette ble støttet laboratoriemessig ved fall i borreliaspesifikke immunkomplekser.
Da er vi inne på det som ble et hovedsatsningsområde i samarbeidet mellom Øystein Brorson og undertegnede, fra tidlig på 2000-tallet: Analyse av borreliaspesifikke sirkulerende immunkomplekser i pasientens serum. Etter vellykket behandling, så vi signifikante fall i denne laboratorieparameteren, som ingen brukte i rutinediagnostikken. Metoden var som nevnt utviklet i og publisert fra USA (3), men ble der bare benyttet i tidligdiagnostikk av Lyme borreliose. Det var ikke, ressursbruken tatt i betraktning, ansett som hensiktsmessig å videreføre immunkompleksanalyser (SE Schutzer, personlig meddelelse 2008). Brorson nedla et stort arbeid i disse analysene. Spesielt var utslagene store ved det vi kaller muskuloskeletale borrelioser. Vi presenterte to postere ved borreliakonferansen i 2008 i Irvine, California, basert på pasientundersøkelser i Tønsberg (10,11). Vi mener å ha dokumentert, som de første noen gang, at det ved Lyme borreliose finnes betydelige mengder vevsbundne, borreliaspesifikke immunkomplekser. Trolig er dette et vesentlig element i symptombildet ved det vi kaller muskuloskeletale borrelioser.
Forskningen ble stanset
Fortsatt er det mye ugjort på dette feltet. Øystein og jeg hadde akkurat startet arbeidet med å lage en oppfølger til 2008-arbeidet med en ny posterpresentasjon til borreliakongressen i Ljubljana høsten 2010, da han ble syk. Dessverre møtte jeg ikke forståelse for at immunkompleksanalysene burde videreføres ved sykehuslaboratoriet i Vestfold etter at Brorson ikke kunne fortsette. Vi var i en observasjonell og erfaringsbyggende fase. Det var derfor foreløpig ikke snakk om noen randomisert studie. Det kan ha ligget bak laboratorieledelsens beslutning om ikke å videreføre immunkompleksanalysene. Disse undersøkelsene ga dessuten ikke inntekter, de genererte kun utgifter. Det var en mager trøst at en av de fremste borrelioseforskere i USA ved 12th ICLB i Ljubljana i 2010, etterspurte en oppfølger av det vi hadde presentert i 2008 i Irvine (G.Wormser, personlig meddelelse 2010).
Allsidig innsikt
Det personlige engasjementet som Øystein Brorson la ned i borreliadiagnostikken var imponerende. Han leste nær sagt alt han kom over av borreliapublikasjoner og hadde et bredt kontaktnett utenfor landets grenser. Artikkelen i Bioingeniøren i 2007 dokumenterer hans allsidige innsikt (2). Det var helt sikkert frustrerende så ofte å møte likegyldighet og avvisning. Fortsatt sliter man med å få fagfolk som burde vite bedre til å innse Lyme borrelioses biologiske kompleksitet. Selv har jeg interessert meg sterkt for tilstanden helt fra 1980-tallet, da jeg opplevde Bodvar Vandviks laboratoriediagnostikk på Rikshospitalet som en spore til praktisk infeksjonsmedisinsk engasjement. Det å komme til Tønsberg og oppleve Øystein Brorsons forskning, fikk meget stor betydning. Sammen tror jeg vi har gitt et bidrag som har kommet norske pasienter til gode. Det er nedslående å lese publikasjoner i velrenommerte internasjonale tidsskrifter som fraskriver Brorson og andre forskeres arbeid innen samme felt, enhver klinisk betydning (9). Det er også en avstand mellom amerikanske og europeiske fagmiljøers synspunkter som oppleves beklemmende.
Oppe i alt dette får man interessegrupper, foreninger og ekstrempraksis som sporer av. Det ene følger det andre.
Spirochetebiologi er komplisert
Det er fortsatt ”miles to go” før forståelse, kunnskap og pasienttilbud er der det burde være. Øystein Brorson kunne sikkert både irritere og provosere, og noen ganger ble hans vurderinger i en klinisk infeksjonsmedisinsk sammenheng litt vel spenstige. Jeg er likevel overbevist om at serien av publikasjoner fra Øystein og Sverre-Henning Brorson har gitt viktig kunnskap som det vil bli bygget videre på. Spirochetebiologi er komplisert. Noen har skjønt det, men det sitter en del personer i fremtredende posisjoner som ikke har det. Den kliniske forståelsen er selvsagt essensiell, men den trenger et diagnostisk fundament i laboratoriet. Utnyttelsen av det vi allerede har er ikke optimal og mer må på plass. Spesielt gjelder det oppfølgning etter behandling. Savnet av en såkalt aktivitetsmarkør med god sensitivitet og fremfor alt spesifisitet, er et problem i den kliniske hverdagen. Immunkompleksundersøkelsene som ble avbrutt var ikke nødvendigvis den endelige løsningen, men min oppfatning er at de har et uutnyttet potensial i bedømmelsen av sykdomsaktivitet og sanering, spesielt ved langtidsoppfølgning.
Les også:
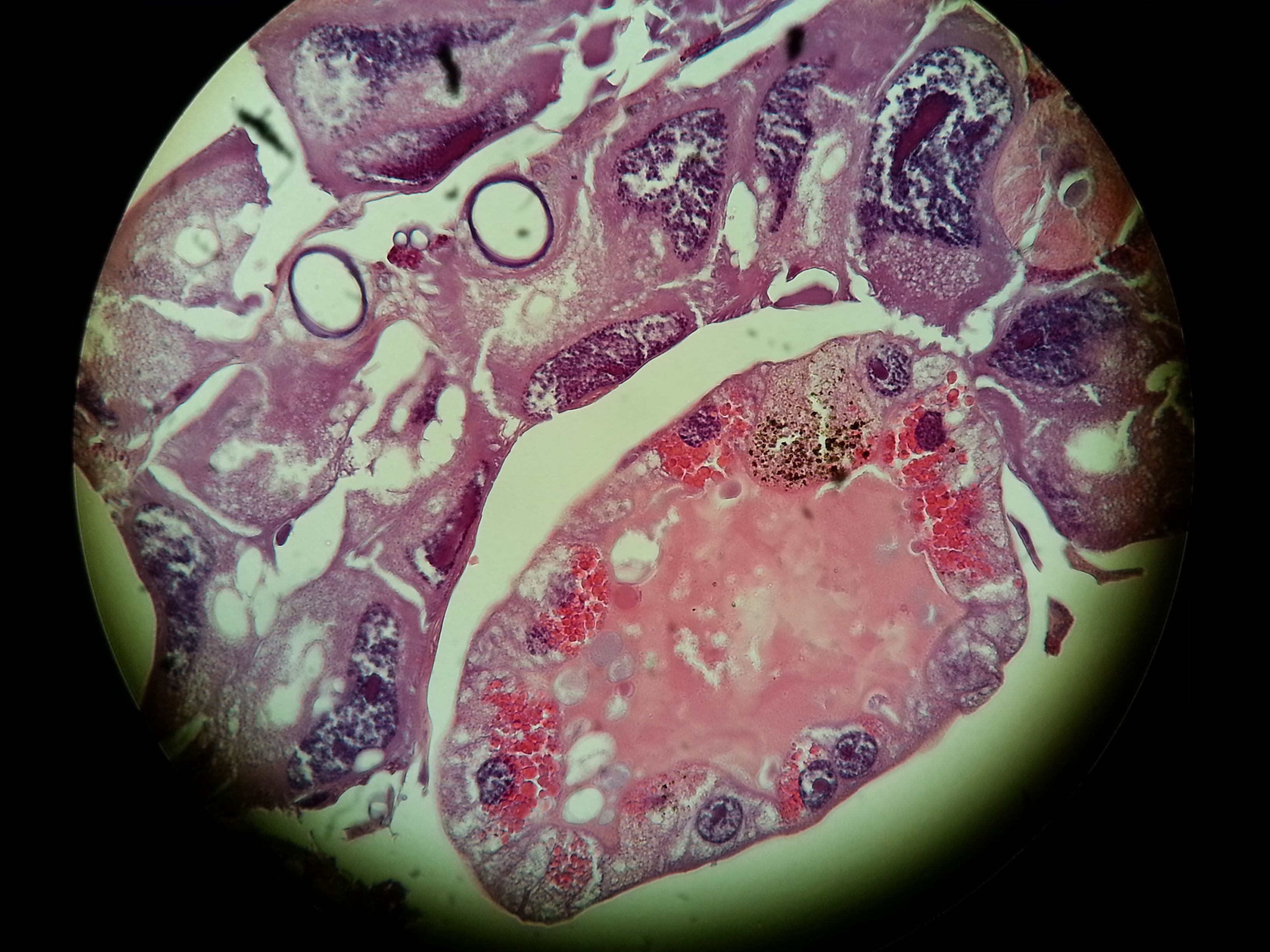
Flåttmidden (Den klassiske: Ixodes ricinus, 8 ben) er trolig det farligste dyr for mennesker i Norden! Livssyklus: egg, larve, nymfe og voksen. Nymfene smittes fra mus. Noen mikrober: 1. Borreliose. Minst fem arter av Borreliaarten. Hyppigst Borrelia burgdorferi. Ofte rødt utslett/ ring rundt bittet. Mikrobene kan gå i dvale! Ny art: Borrelia miyamotoi. “Ikke utslett”. 2. TBE (Tick-borne encephalitis). Hjernebetennelse. Vaksine! 3. Rickettsia helvetica. Bakterien kan gi hjerterytmeforstyrrelse. 4. Neoehrlichia mikurensis. Bakterien kan gi influensaliknende symptomer og blodpropp (ofte). 5. Bartonella henselae. Bakterien fra flått til katt til menneske. Hjerteklaffbetennelse, hjernehinnebetennelse. 6. Babesia. Parasitt- likner på malaria. Ødelegger blodlegemer. Ofte hos hunder og kveg. I mikroskop: Maltese crosses in erythrocytes.
I helsevesenet er der stor uenighet om hvordan man skal behandle pasientene som er angrepet av borrelia. Det offentlige helsevesen er restriktiv med å utøve lengere penicillinbehandlig, mulig dette uten skikkelig vitenskaplig vurdering!
Hvordan man påviser borrelia er også uklart/ usikkert. Det finnes for dårlige påvisningsmetoder!
Trolig vet man ennå for lite om påvisning av borrelia og også om behandlingsopplegg.
Borreliabakterien går ofte over i cysteform (“spheroplast”), som trolig kan være vanskelig å angripe med medikamenter.
Tenk på: Det tok f.eks. lang tid før man kunne påvise TBC-bakterien, Denne bakterien har langsom intermiterende metabolisme, og her mot denne bakterien bruker man langtidskombinasjon av medikamenter. Selv om man mener at borrelia er sensitiv for kortidsbehandling med penicillin, kan mulig langtidsbehandling/ kombinasjon av medikamenter være riktig i en del tilfeller, når bakteriene er såpass spesielle (se også trippelbehandling ved helikobakterpåvisning i magesekk- mot mavesår. Les historien!).
Leger må ikke være så skåsikre!! Historien har flere ganger vist at det var feiloppfattning på et tidligere tidspunkt!
 |










Interview with professor Laane about the suppression of microscopy for Lyme diagnostics
Written by Huib
Around 2003 the WHO encouraged research into microscopy as a direct test for the Borrelia spirochete, the pathogen causing Lyme disease. When a promising new and simple technique was discovered in 2013, it was however violently attacked. Not on the science itself, which is the normal procedure in science, but personally. Now retired professor microbiology Morten Laane was fired after he gave a lecture at a scientific conference in 2014. Moreover, his laboratory was closed down, the website of the scientific journal was hacked and the article disappeared. An exclusive interview.
“If experts treated airplane accidents in the same manner as an average medical scientist studies disease, I would book my next travel to the USA by ship.” Professor Laane
(c) courtesy of Under Our Skin
Who is professor Laane?
Born in July 1940, in the small city of Toensberg, Morton Laane grew up during the second World War. “My mother visited her sister in the city of Bergen the ninth of april 1940 the day war broke out in Norway. They survived the severe attacks by the German warships. My mother travelled along the coast by a Norwegian local ship to the small city of Toensberg where the family lived close to the Oslo fjord. This was not a very smart idea, as several ships were attacked and destroyed by German submarines.
My father was in Finmark, the arctic part of Norway, together with a substantial number of Norwegian soldiers as a medical officer. When I was born, my mother, who had professional training in handling weapons, sat alone with a hidden gun in a small flat close to the German headquarter across the street. When the free artic part capitulated a couple of months after the start of the German invasion, he was first arrested by the Germans, later released and went back to Toensberg.
In 1947 my father showed me how to detect the Syphilis spirochete by very simple microscopy. Numerous sailors lived in this city known for its substantial commercial fleet. Back then, Syphilis infection was not uncommon in sailors.
My father had a small, old Leitz brass microscope of high quality. A tiny sample from the patient was mixed with an equal part of drawing ink on the glass slide made for microscopy. Drawing ink consists of extremely tiny black particles (coal). They do not penetrate into the bacteria. Normally they are almost invisible. Light pass through the unstained bacteria against a total black background.
This started my interest for microscopy. Later my father specialised in psychiatry. He had no use of his microscope and I got it as a gift. Looking back, almost everything in my life started as a hobby.
I became scientific assistent in general experimental genetics. My boss, Dr. Øistein Stromnaes worked with the fungus Penicillium. Nobody had seen its chromosomes before, but I discovered a simple method to count them in the light microscope.
So I was offered a research fellowship a the University of Bergen, I continued my research there and my PhD dissertation took place in 1971. The committee evaluated my theses as very good and suggested that I might have the qualifications of a personal professor position for life time and further develop new methods in genetics.
One of my discoveries regarding Penicillium brought me in contact with Lynn Margulis, then Lynn Sagan, wife of the famous Carl Sagan. Her research on cellular evolution and endosymbiosis led to the understanding that the energy-converting organelles, the mitochondria and chloroplasts, are actually bacterial symbionts living inside eukaryotic cells. This discovery earned her the reputation of being the most famous scientist in evolutionary biology after Charles Darwin.
My discovery was connected with her spirochete research, which focused on the symbiotic nature of the relationship between spirochetes and their hosts, in particular the noted ability of these bacteria to form dormant “round bodies” that are capable of reactivation. Nobody in the world knew more about spirochetes than Lynn.*
Later I discovered a somewhat similar structure in the slime mould (Physarum) which was much used for experimental research. I got in touch with Professor Ivar Giaever, a Nobel laureate in Physics and we cooperated for many years supervising Master and Ph.D. Students.”
Microscopic Lyme diagnostics
Microscopy is considered the Golden Standard in diagnostics for Syphilis. Given his background and expertise in microscopy, it made sense to Laane to try and find a method to detect the Borrelia in infected blood.
Laane: “My coworkers and I had published a series of papers in the Norwegian journal ‘Biolog’ regarding a problematic sheep disease called “alveld”. The papers contained unusual and spectacular images of possible toxic blue green algae (bacteria) that were suspected to be connected with this disease.
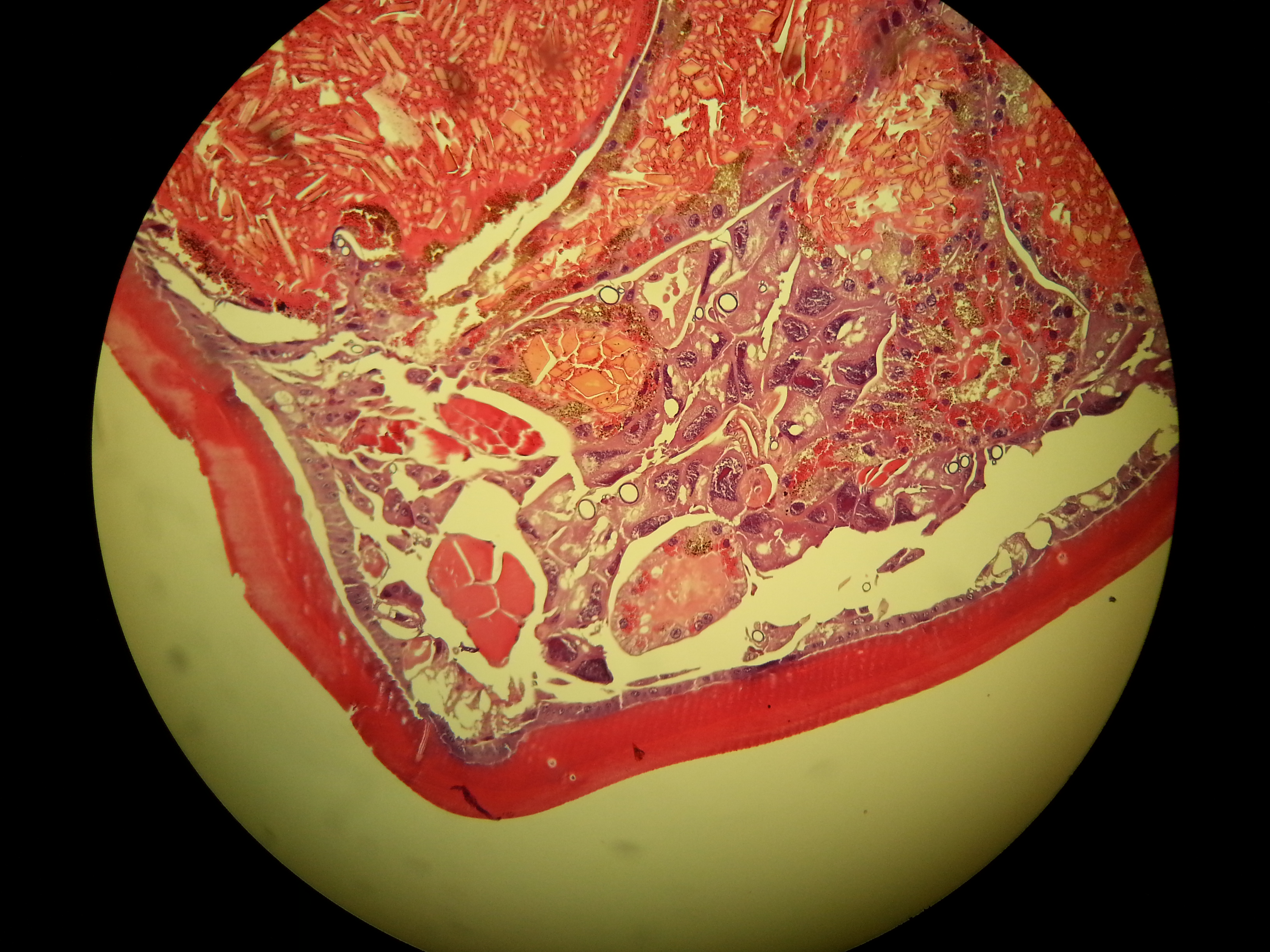
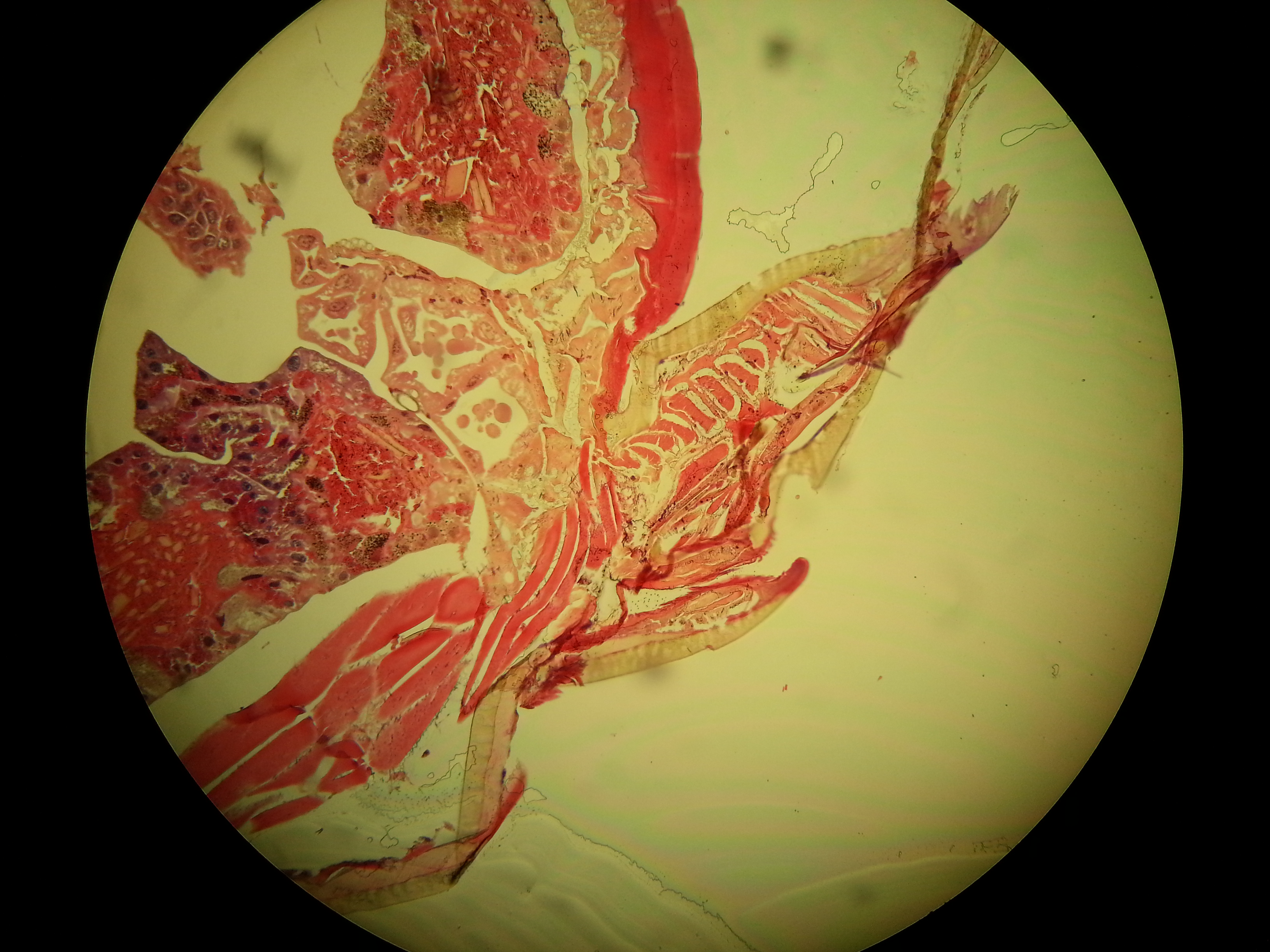
The Biological Institute then asked for cooperation regarding Lyme infections in order to compare microscopy and molecular tests. The Institute was responsible for administration regarding formal permissions to do medical research. It turned out that no reliable data were obtained from the molecular studies. The institute was responsible for this part. Microscopy showed, however, characteristic spirochetes in a number of patients together with other organisms such as Babesia.
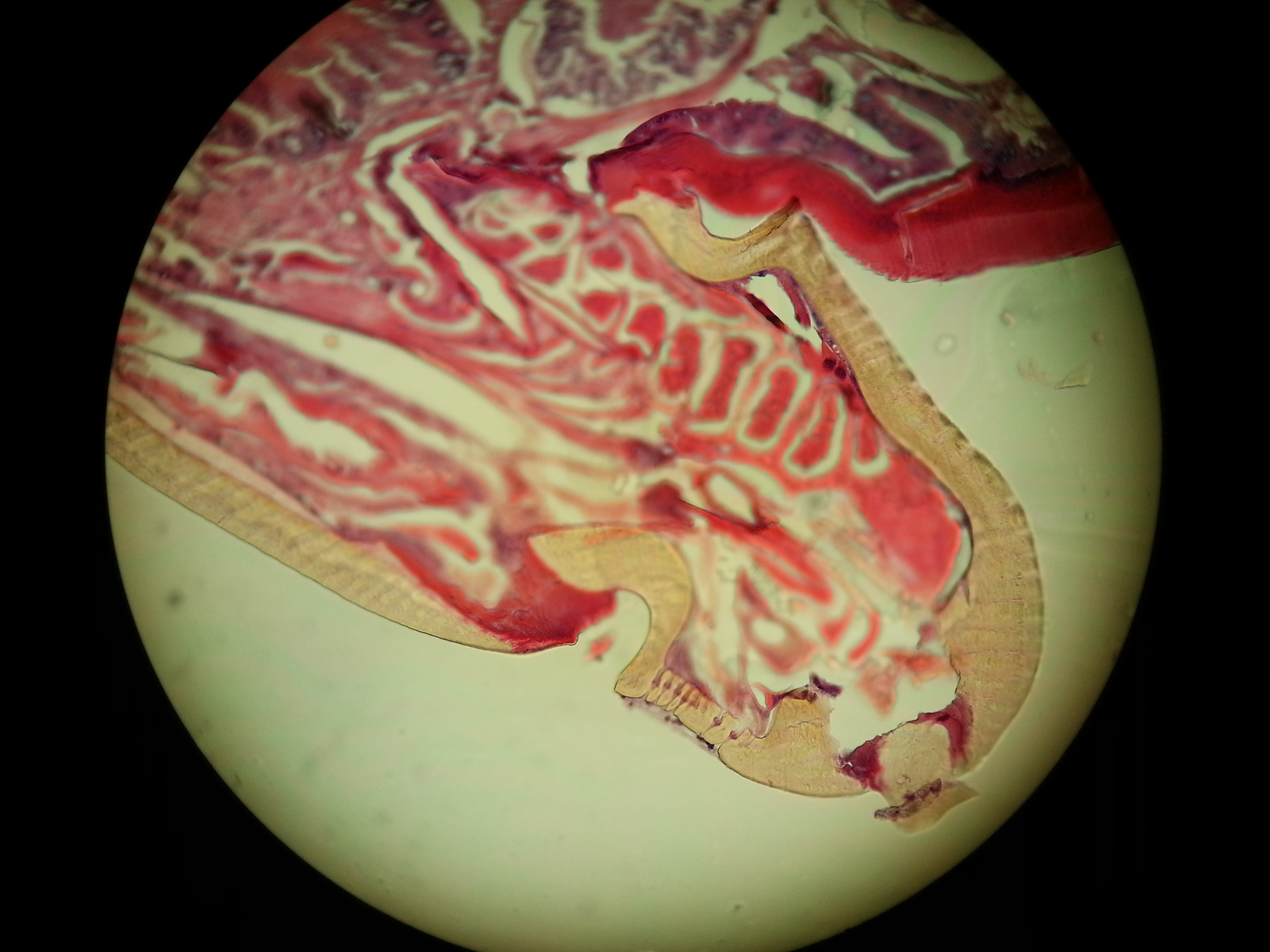
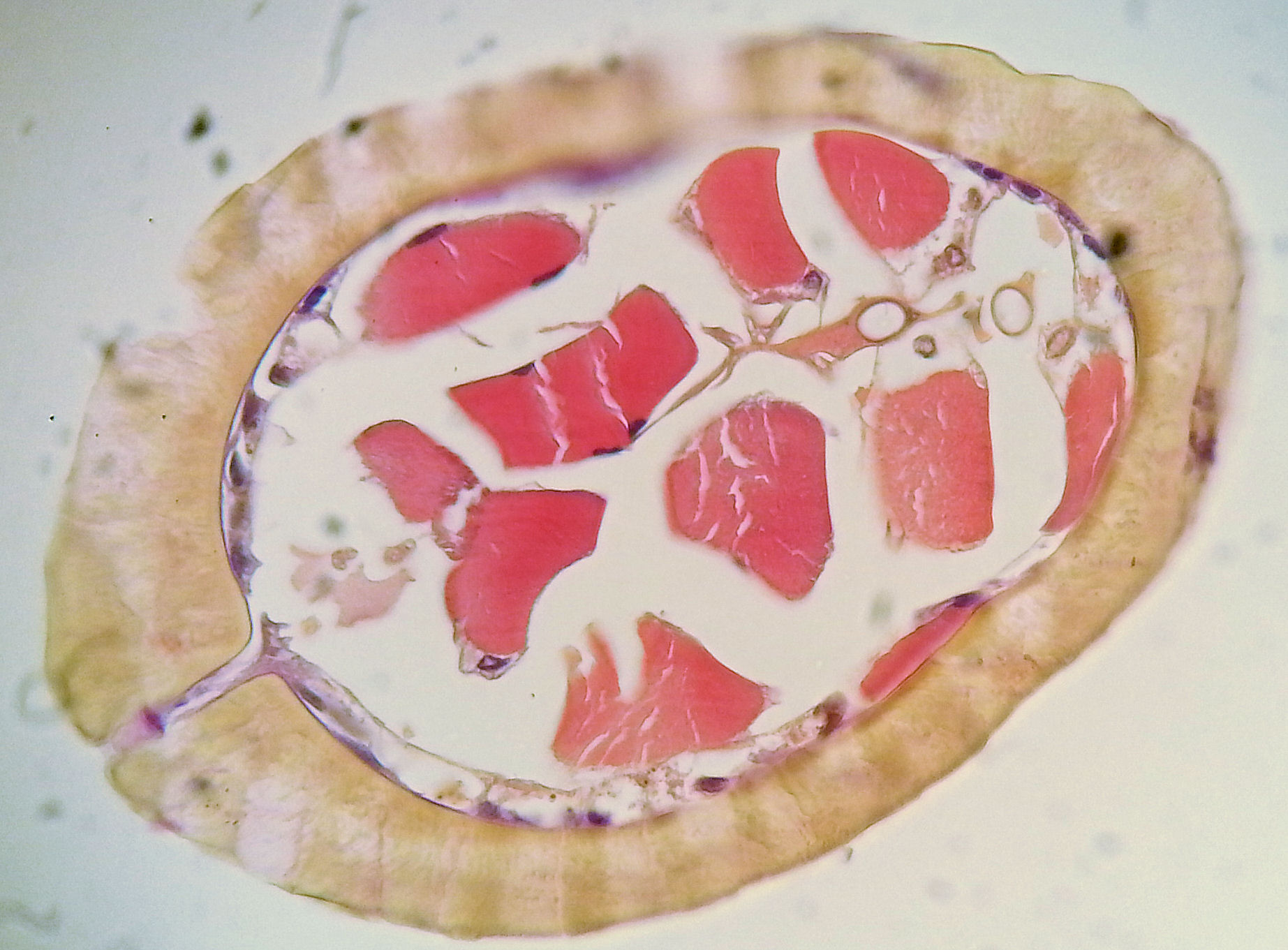
The syphilis and Borrelia spirochetes share many properties. They cause permanent infections in humans which cause long-lasting, multi-stage diseases. They exist in more than one form – sometimes in the long spirochete form, but also in a round “cyst-like” form. The spirochete form can be made visible by simple methods and observed with a microscope.
Borrelia spirochetes in dry smears and in isotonic solutions appear as very thin cells, only 0.2 micrometers wide, and as very long – in the range of 50 to 100 micrometers. These are visible above the resolution limit for light microscopy – due to what we call light interference – by slight defocusing. In dry preparations, a focus error of more than 1/1000 mm renders them invisible under the microscope. In wet preparations, the cells swell substantially.
My colleague and I published the results of our part of the project due to our firm belief that microscopy is useful for detecting these infections. Beforehand we were assured by the Institute that formal permissions were granted by the health authorities. It turned out that the Institute, somehow had forgot to point out in a formal enough manner that a substantial part of the project included microscopy by us!
Our project leader was educated as a medical doctor, and had later became a biologist. He was also Head of the Institute to which the project was connected. We, my colleague and I, got a copy of the first page of the application accepted and signed by the Health authorities. We did not, unfortunately, see the entire application before it was too late, as the project description was incomplete in that it did not express without any doubts that about half of the project involved extensive use of microscopy to analyze samples.
The project leader knew of my cooperation with Oeystein Brorson, the extremely clever technician who was able to grow Borrelia from infected blood samples. We had agreed that the application should be written to state that extensive microscopy was needed for the project as a way to confirm the results of molecular tests.
The Institute received around 2 million euro (NOK 20 mln) and bought two DNA machines. The test project was thus an official Institute project, not an application by a group of three scientists. In hindsight, we should have asked to see the complete application, but we did not and went on the trust for our project leader. This turned out to be a mistake, as we were later blamed for not reading the regulations for medical research and additional legal papers.
The trust that caused us to not read the full application was labelled as “intention,” to mean we intended to subvert the regulations when we embarked on this project. This is simply not true.
Silenced for speaking
After publishing the 2013 article ‘A simple method for the detection of live Borrelia spirochetes in human blood using classical microscopy techniques’, professor Laane was invited to give a lecture at the 2014 Norvect conference in Oslo. An English patient saved the pdf, so you can still read it, via the link provided.
I was present at that conference and still remember how nervous he was. The reason was that several medical professors complained to his university. He was threatened with losing his job, if he would speak at the conference.
In fact, he did not literally speak – as you can see in the movie below – but used performing arts to show the slides of the spirochetes. Professor Laane was fired anyway and his laboratory was closed down.
Laane: “As for being forbidden to speak, Waldemar Broegger, a Geology professor in the late half of the nineteenth century was forbidden to speak about Charles Darwin’s evolution theory. Lynn Margulis was originally ridiculed for her theories on the evolutionary origins of mitochondria and chloroplasts and later received numerous awards for this discovery. As both of these scientists were found to be right and later became famous, I feel I am in good company.“As for being forbidden to speak, a Geology professor in the late half of the nineteenth century was forbidden to speak about Charles Darwin’s evolution theory. As this professor Waldemar Broegger later became famous, I am in good company.
The 2013 publication of ‘A simple method for the detection of live Borrelia spirochaetes in human blood using classical microscopy techniques’ in the journal Biological and Biomedical Reports resulted in much opposition by conservative medical doctors and some scientists, most of whom had little or no microbiology experience working with spirochetes in a laboratory environment.
The article and research was criticized because the cellular objects we were observing were presumed to be “artifacts,” meaning objects of some other origin that just magically appeared in our samples. It’s extremely important to point out that all of our principal research was performed under highly controlled conditions, and our results were confirmed using more than one microscopy method. The critics of our work have yet to explain how these supposed “artifacts” we observed were able to reproduce and even move like spirochetes, which we observed them doing, and even more importantly, the critics have failed to explain how an “artifact” could possibly contain nucleic acids from Borrelia.
Yet, in that same year Dr. Alan MacDonald found out independently the same as me regarding how to detect chronic Lyme infections in human blood. Before this the assumed borrelia bacteria had been found by a Norwegian microscopist, who had an extremely ill son from Lyme.
MacDonalds arguments in these two videos (part one and part two) are brief, but very much to the point. He has later developed methods to detect single Borrelia bacteria direct in a microscope slide by exact molecular methods.
Oeystein Brorson is also mentioned by MacDonald. He was the researcher who grew all known strains of Borrelia in Norway, sent me samples and cooperated with Lynn Margulis and me, until he got disabled due to disease and had to leave his job.
After my lab was closed down, also the website of the scientific journal that published our article was so severely hacked that it stayed offline for three years. Once it came back up, our article had dissapeared.
The hacking of the Journal ‘Biological and Biomedical Reports’ seems to be done with a person knowing more than my closest enemies. And was someone with access to a quite advanced compilator system. Why this was done might well have been political or personal prestige.
I have never seen this happening on any topic in science before.”
Proof or propaganda?
In 2016 the Norwegian Health Department (FHI) published the study ‘Validate or falsify: Lessons learned from a microscopy method claimed to be useful for detecting Borrelia and Babesia organisms in human blood’. It stated that “microscopy by the LM-method identified structures claimed to be Borrelia- and/or Babesia in 66% of the blood samples of the patient group and in 85% in the healthy control group”.
The TV2 reporter in the infamous documentary ‘Deceit or Borrelia’ misquoted this sentence by claiming that “it was proven that Dark Field microscopy produces 85% false positives”.
There are however suspicions that the Norwegian study was set up to discredit professor Laane’s work, using contaminated blood.
Laane: “Officially, on their website The National Institute of Public Health claimed that the only known case of Babesia in Norway was a veterinarian that have had his spleen removed, and else that Babesia was unknown in the Norwegian population.
But I found a faked sample of Babesia. It was blood from a cow (or ox). It was mixed with human blood from a socalled control person and sent to me by mail.
Of course, this sample clotted impossible to see anything in the sample by microscopy except lumps of erytrocytes and fibrine fibers. If I had got the original sample unmixed, I would have found them at once. The FHI showed me a few images from a preparation they had made themselves, BEFORE it was mixed with human blood. The Babesia images there were the same as I found in several so-called control samples.
When I showed them, they looked a little worried – like school children not telling the truth to their teacher – but they would not admit that control samples contained Babesia merozoites.”


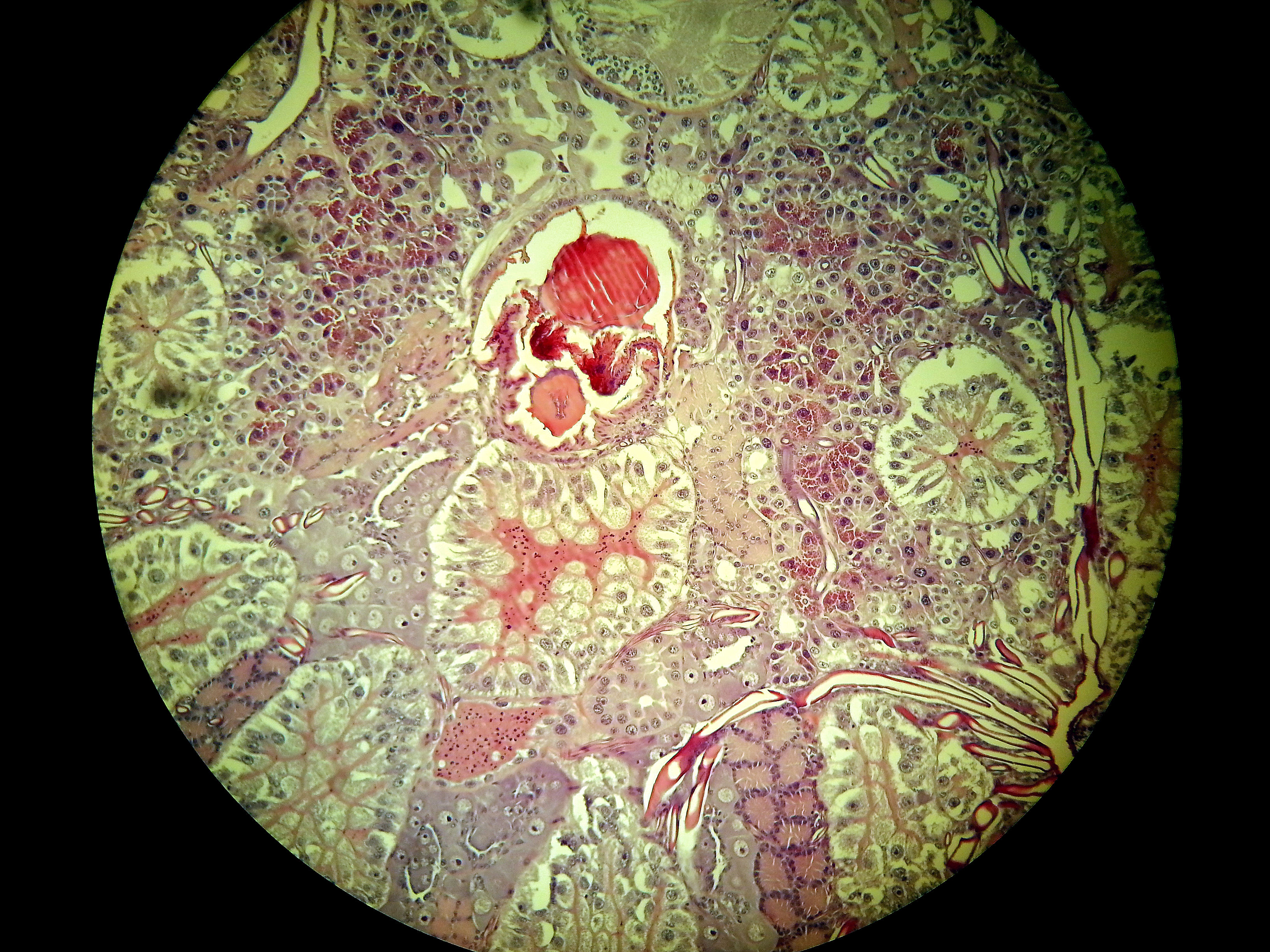
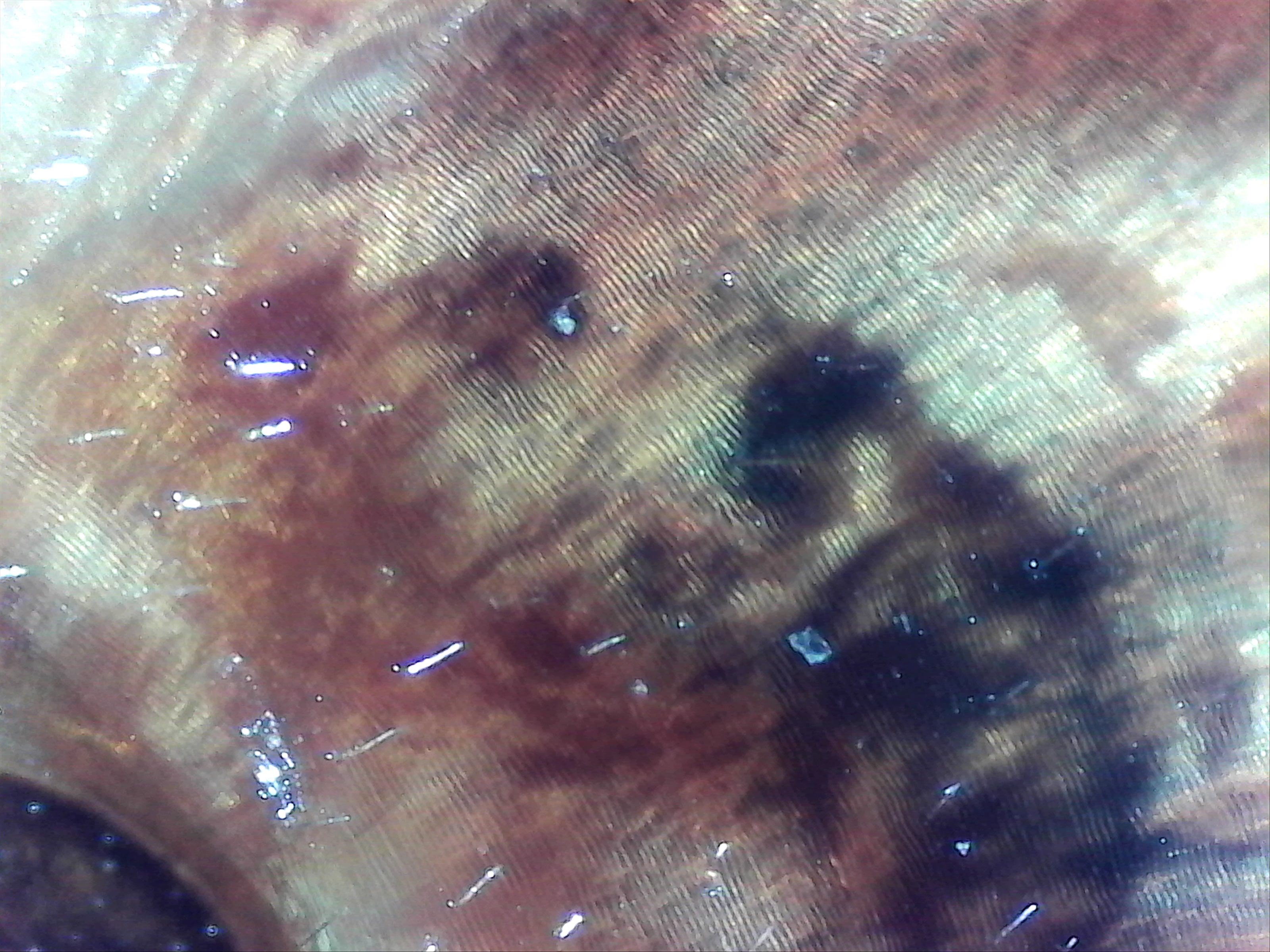
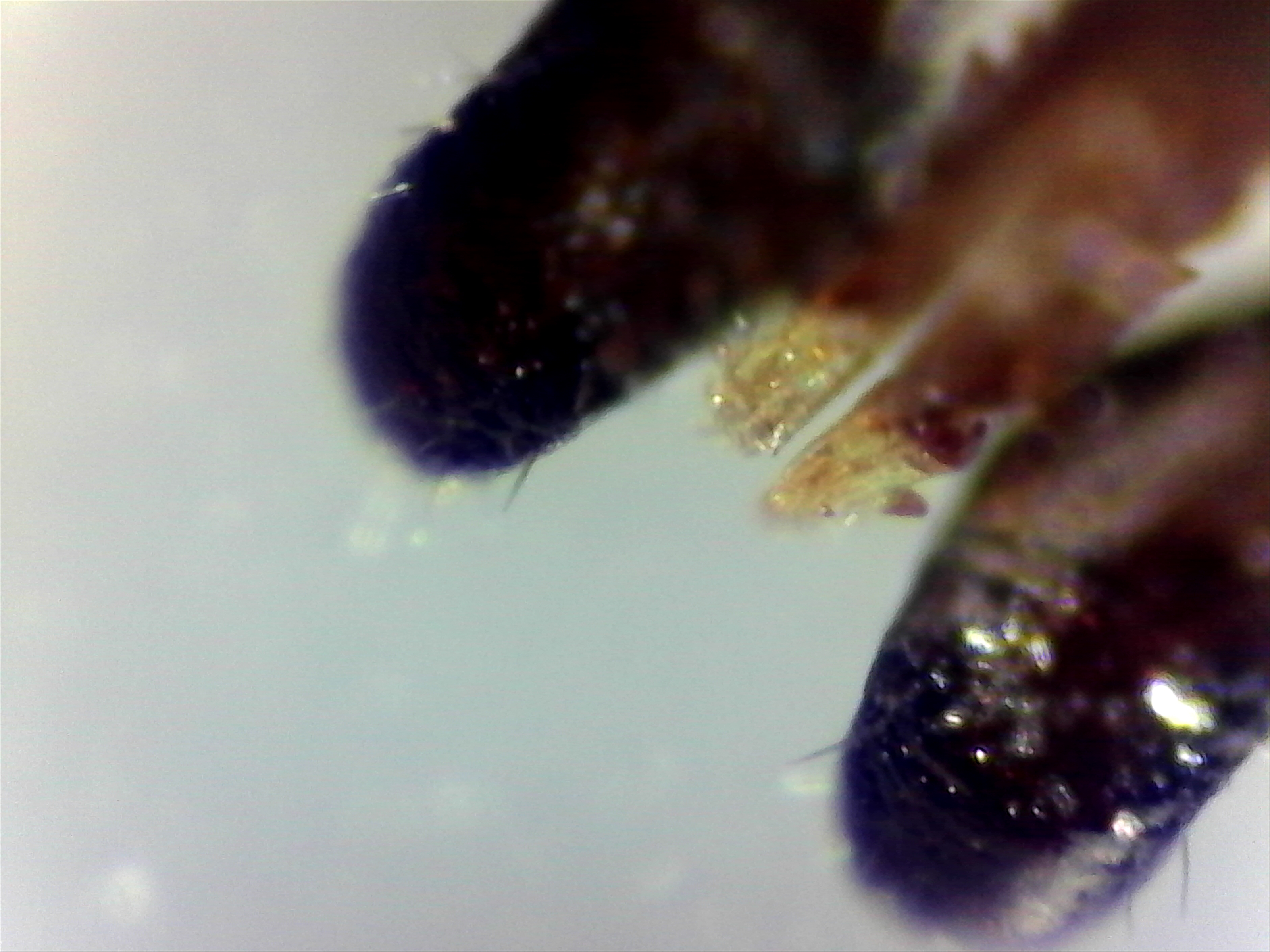
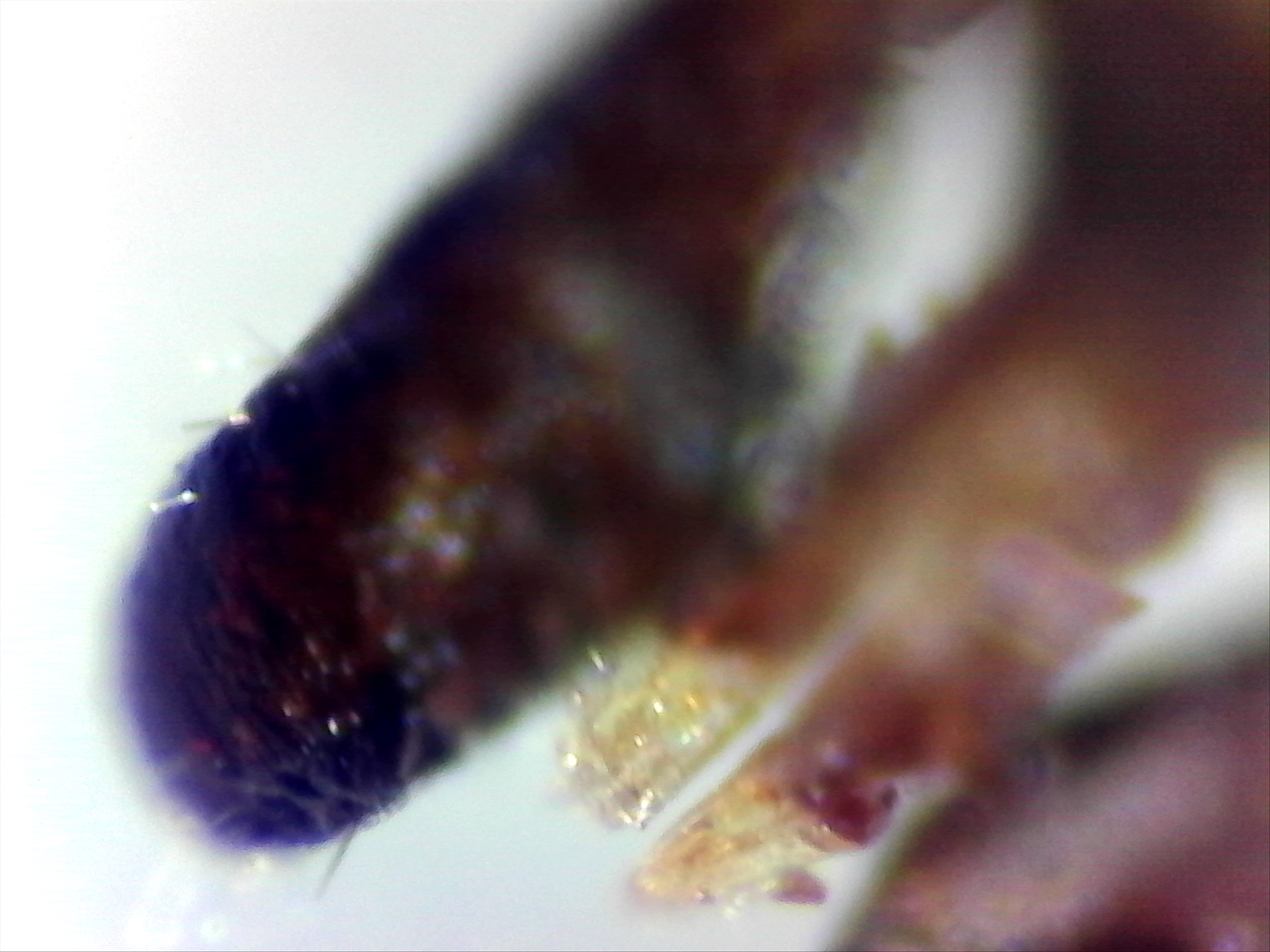
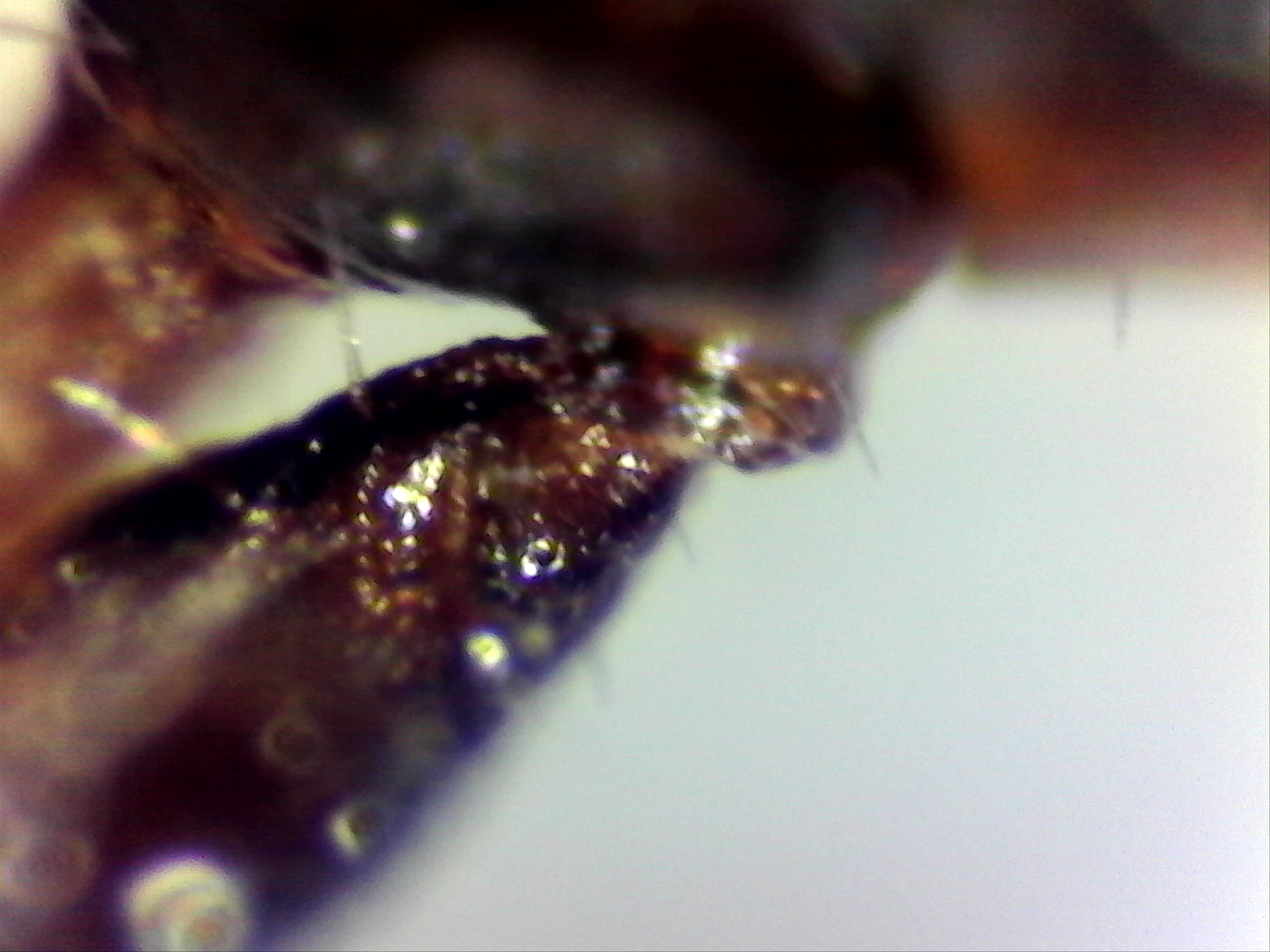
Image left: a Borrelia stained with the Mysterud-Laane method, blue color. Image right: live biofilm of Borrelias developing in a mixture of blood and sodium citrate (this patient was tested positive also by molecular methods by American laboratory).
Serology
In the introduction to their 2016 article, the FHI authors also state that Lyme serology has a 70-90% sensitivity in the earliest stages and a sensitivity of almost 100% in later stages, which suddenly seems to become the new mantra in several countries. This seems to have been taken from a 2016 article written by IDSA and CDC authors, which was criticised for using circular logic.
Laane: “A recent report presented in Norwegian newspapers claim that inaccurate science, especially in medical topics, is common. Norwegian Professor Oeyvind Oesterud has written several short articles in Aftenposten, Norway’s largest newspaper about science and popular science papers.
He points out that false conclusions are favoured by both journals and media on the criteria that discoveries should be spectacular. Unless they are not, they are not accepted. Also the official evaluation system for research grants favours this. Many of these discoveries can not be repeated. But it generates much money for the universities.
Such scientists believe in accepted science. Any deviation shown by experiment may be interpreted as incorrect or false. One may wonder why they publish at all. Regarding deviating disease data they are often neglected – according to what the medical scientist was taught as a student by his professor. The deviating results are never studier further and ignored as “errors”. Up to about half of recent medical papers may contain this.
The result is delayed progress, sometimes with big consequences for severely ill patients. Patients that could be saved. Disease problems are very complicated and there is need for research listening to what both the patients tell and meticulous analysis of unexpected data.
As a final thought: travel by modern airplanes is now very safe. If experts treated airplane accidents in the same manner as an average medical scientist studies disease, I would book my next travel to the USA by ship.”
Exception or a pattern?
The European Union has recently provided a 2 million euro grant to a cooperation of three parties to develop a better Lyme test, as the current one is considered imperfect. At best.
So why are there several indication of the active repression and sabotage of new, better and direct ways to diagnose Lyme? Is professor Laane’s story unique or showing a doisturbing pattern?
“This never happened before on any topic in the history of science in Norway”, Laane said in his interview with the makers of ‘Under Our Skin Emergence’. Yet also in other countries scientists have been attacked for working on promising new and direct Lyme tests.
In 2014, French lab director Schaller was fined was fined with paying 280,000 euro to the government and was sentenced to nine months in jail. Also in 2014 the American Centers for Disease Control and Prevention (CDC) publicly attacked the credibility of Advanced Laboratory Services, which had developed a culture-based test for Lyme disease diagnosis. The basis for the CDC’s attack has since been proven wrong, yet the CDC has never retracted the article in which the errant criticism was made.
A direct and ‘no false-positive’ DNA test for Lyme was no longer made available to the general public, after its inventor was fired from a Connecticut hospital in 2010. And recently media attacked the tests of specialised labs in Germany, using undercover reporters and twisted patients’ stories, claiming they were either not ‘FDA approved’. As professor Ahern explained in her recent interview, none of the tests promoted by the CDC or your national Health agencies are ‘FDA approved‘.
The next interview with Dr. Lee will look into what happened around the development and public accessibility of the DNA diagnostics mentioned above. It will be published very soon.
* Professor Laane and I will work together on a future article about the work of Lynn Margulis, as too few people seem to have heard of her important work.
Interviewer / author: Huib Kraaijeveld
Call to action: ‘A Matter of Dignity’
This interview has been nearly 9,000 times. However, due to lack of funding the On Lyme Foundation ceased to exist as a non-profit entity. Soon this website will no longer be available online.
With your help the most important existing interviews with caretakers, doctors, scientists and legal professionals can be published in a new book called ‘A Matter of Dignity’. Previously unpublished materials and new interviews with professionals taking a stand for the human rights of people with an ME diagnosis will also be included in it. From an ethical and social point of view, both groups suffer the same fate.
Can you help achieve that goal by joining the Indiegogo campaign and by sharing this message?





 Views Today : 67
Views Today : 67
